Pelvic Organ Prolapse
Introduction
Pelvic organ prolapse (‘prolapse’) describes a lump or bulge in the walls of the vagina. This is caused by a pelvic organ (bladder, uterus, or bowel) moving down in the pelvis. As these organs move down, they push on the soft skin of the vaginal walls, causing them to stretch and curve out into the vaginal canal. This causes symptoms of ‘something coming down/ falling out’ or a feeling of heavy pressure in the vagina. This bulge may be felt inside the vagina or seen on the outside the vagina. Women may describe it as a pink coloured lump, which can be a similar size to an egg or small orange.
A prolapse can be mild and asymptomatic, or it can be severe, causing symptoms and affecting your daily life. Prolapses are extremely common; affecting 1 in 3 women.
What is a Prolapse?
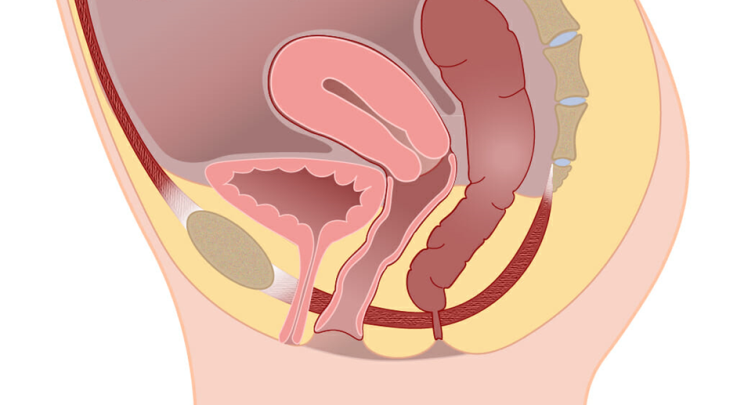
The picture below shows a side view of a normal female pelvis (without any prolapse). As well as showing the three pelvic organs in their original positions. It also shows the pelvic floor muscles sitting underneath them.
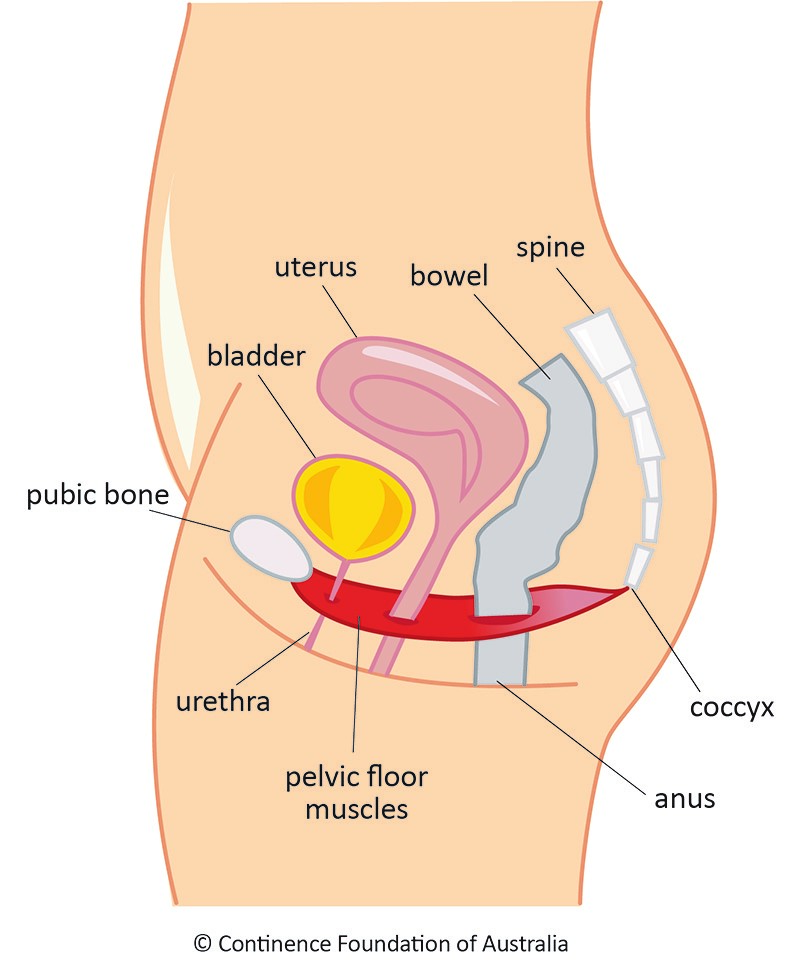
The pelvic floor muscles and ligaments (strong fibrous connective tissues) help support the pelvic organs and keep them in place.
When the muscles are weak, and the internal ligaments are overstretched, the support to the pelvic organs is compromised. These organs can move downwards resulting in a prolapse.
The terms used to describe a prolapse are often confusing. You may have been told you have a vaginal prolapse, or a pelvic prolapse. These are generic umbrella terms that describe a prolapse of any one of the three pelvic organs. Alternatively, you may have been told that you have a bladder prolapse; also known as an anterior wall prolapse, an anterior prolapse, a cystocele, or a urethrocele. You can also have a bowel prolapse; known as a posterior wall prolapse, a posterior prolapse, or a rectocele. Physiotherapy treatment for a prolapse is the same, regardless of the organ that has shifted position.
Common Types of Prolapse
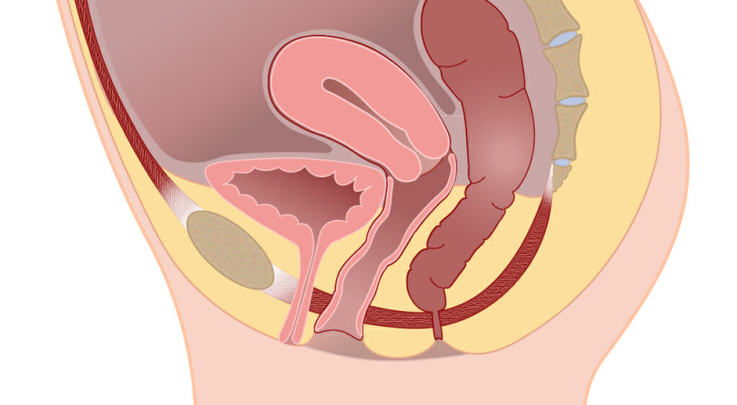
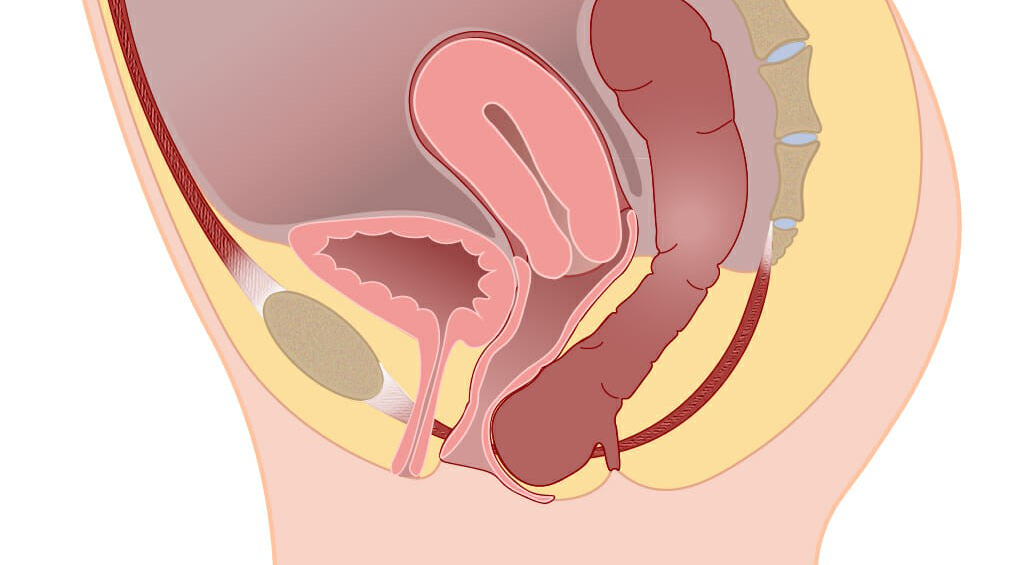
Anterior Wall Prolapse / Cystocele / Bladder Prolapse
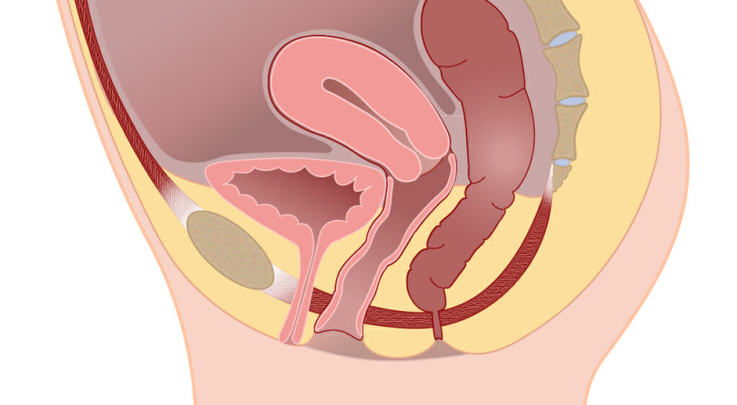
In these pictures you can see that the bladder has shifted down in position. Part of the bladder is putting pressure on the soft skin of the vaginal wall, creating a bulge just inside the entrance to the vagina. This picture shows a mild to moderate prolapse. As a prolapse becomes more severe, the bulge becomes larger and moves further down the vagina.
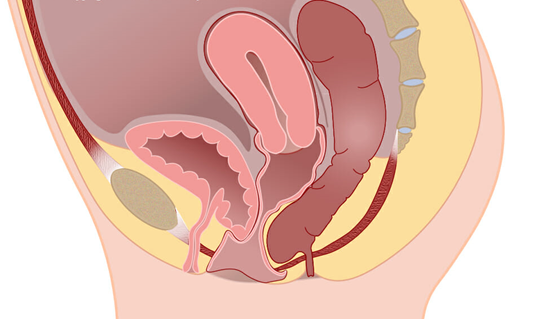
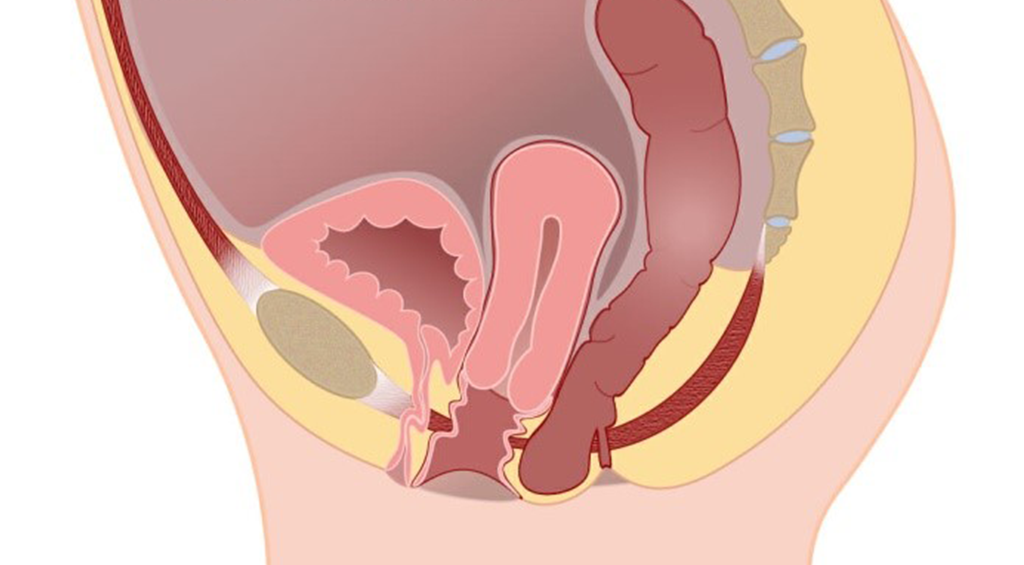
Posterior Wall Prolapse / Rectocele / Bowel Prolapse
These pictures show how the bowel has shifted position. The bowel exerts pressure onto the vaginal skin, creating a bulge inside the vagina. The bowel can also push down on the skin between the vagina and the anus (the perineum). This creates a sense of “heaviness” or “pressure” which can either be felt inside the vagina, or the perineum, depending on the individual’s anatomy.
Uterine Prolapse
These pictures show how the uterus has shifted downwards. The picture shows a moderate uterine prolapse. When severe, the uterus moves further down the vaginal canal. The uterus is in the middle of the pelvis and firmly attached to the bladder and bowel on each side. Because of this, the uterus can pull on the bladder and bowel as it descends making it possible to get a degree of bladder and bowel prolapse with a uterine prolapse.
After a hysterectomy, women can still have a prolapse in the middle of the pelvis. This is called a vaginal vault prolapse. Although the uterus has been removed, the top of the vagina can still move down and prolapse for a “vault prolapse”.
Causes of Prolapse
- Pregnancy and childbirth – this is the most common factor, especially with a difficult vaginal delivery, although women who have had a caesarean section can also be affected.
- Obesity/ being overweight – body weight is held up by the pelvic ligaments and pelvic floor. Any extra weight in this area puts a stretch and strain on these supporting structures, weakening them.
- Heavy lifting – when you lift anything heavy, the weight is transferred inside the body. This internal strain weakens the structures supporting the pelvic organs.
- Having a family history of prolapse – this may be due to inheriting a more flexible type of collagen which is not as sturdy and supportive as other types.
- Menopausal changes – menopause causes a decrease in oestrogen in the blood stream. The tissues in the pelvis need the oestrogen to stay healthy. When oestrogen levels fall then the tissues are no longer as strong and healthy.
- Constipation – pushing and straining on the toilet cause a direct downward pressure onto the pelvic organs. This causes a lengthening and weakening of the support structures.
- Chronic cough – coughing causes the diaphragm (the structure under your lungs) to move downwards suddenly and forcefully. This downward pressure of the diaphragm causes a downward push onto the pelvic organs. Over time, with a chronic cough, this repeated pressure causes a strain on supporting structures.
- Previous pelvic surgery – if you have already had an operation to repair a prolapse (or have had a hysterectomy) then your risk of developing a prolapse in the future is increased.
- Aging – over time, pelvic ligaments lengthen and stretch. This is part of a gradual aging process that affects the whole body. Over time, many structures in the body may not be as tight as they originally were. Gravity causes a constant downward pressure on our bodies. As time goes on, the structures inside our pelvis move downwards in response to gravity over time.